A Practical Guide to Travel-Related Disorders
While travel can be fun, it can expose you to obvious as well as hidden hazards, possibly causing illness or exacerbating existing health issues. Lack of sleep combined with stress, dehydration, increased exertion levels, musculoskeletal stresses and a change in medical-care delivery systems could have an impact on the traveler.
A few disorders, however, are actually caused by the process of getting from one place to another around the globe.
The four most common conditions caused by travel are:
- Jet Lag
- Motion Sickness
- Deep Vein Thrombosis
- High Altitude Illness
The following sections of this guide provide a summary of the causes and symptoms of each condition as well as tips for prevention and instructions for treatment.
— Contributors —
James M. Chimiak, MD
Petar Denoble, MD
What is Jet Lag?
Long-distance travel in which humans cross several time zones in a short time can cause what is commonly known as jet lag, also called rapid time zone change syndrome or desynchronosis. This condition results from your circadian rhythm — your internal clock, which is attuned to the day-night cycle at your departure location — being out of sync with the day-night cycle at your destination with little or no time to adjust.
Jet lag primarily affects air travelers because of the greater distances and time zones covered in a relatively short time. Boaters may have some difficulty with this condition if they do not make regular accommodations as they travel across the globe.
Symptoms of Jet Lag
Feeling sleepy, hungry and alert at the wrong times are common symptoms of jet lag, which may affect your social life and your ability to work, exercise or sleep. Fortunately, your internal clock will synchronize with your new environment within a few days. The more times zones you cross, the more intense your symptoms are likely to be and the longer they will take to diminish.

Prevention and Treatment of Jet Lag
A few days to a week before your departure, try to gradually move your bedtime to what it will be at your destination — i.e., if you are traveling east, where night comes sooner than at your departure location, go to bed one hour earlier than you usually would for as many days as the number of time zones you will travel through. To make it easier to fall asleep early, avoid coffee, tea, chocolate, alcohol, and exercise for three to four hours before your new bedtime. Then wake up earlier in the morning and try to catch some sunshine to help your body's internal rhythm adjust. If you are traveling west, you should do the reverse routine — gradually go to bed and wake up later in the days leading up to your departure.
Jet lag may be exacerbated by poor sleep during an overnight flight. Falling asleep on a plane can be difficult for several reasons. During sleep, your body temperature falls, and the activity of some hormones changes. This process usually occurs at a similar time every day, prompted by changes in surrounding light and noise. With the onset of darkness, the pineal gland in the brain starts to secrete melatonin, known as the 'hormone of darkness.' Melatonin helps the body fall asleep and stay asleep, but it is not strong enough to do so on its own.

To sleep well during a flight, it is important to avoid excessive consumption of caffeine and alcohol. Caffeine may prevent you from falling asleep, and alcohol will prevent you from staying asleep and experiencing normal restorative stages of sleep. The use of earplugs and an eye mask to reduce noise and mimic darkness may also help.

Upon arrival at your destination, stay active during daylight hours, and go to bed in the evening at your usual time. You might also consider taking melatonin before your bedtime for the first few days at your destination. In the morning, going out in the sunlight will help your circadian rhythm adjust. If weather prohibits exposure to sunshine or if you are traveling from a summer climate to a winter one, try to start your morning with exercise at a gym or swimming pool.
If these measures are not sufficient, try taking between 0.3 mg and 1.0 mg of melatonin 30 minutes before your bedtime.
About Melatonin
Classified as a food supplement, melatonin is available without a prescription and is not regulated by the U.S. Food and Drug Administration (FDA). The amount of active hormone in one dose may vary slightly from what is declared on the box, and response to melatonin varies individually. Excessive melatonin may interfere with your sleep. Avoid taking more than 3.0 mg at once, as too much melatonin can cause headaches, nausea, dizziness or irritability.
Considered nonaddictive and safe for short-term use, melatonin can interact with certain medications, however, including anticoagulants, immune suppressants, diabetes medications, and birth-control pills. If you have any health conditions, check with your doctor before using melatonin.
Refrain from activities that require alertness — such as driving, boating or diving — for four to five hours after taking melatonin.
Tips For Boaters About Jet Lag
Observe members of a boat crew for evidence of drowsiness and jet lag, as its effects will be cumulative if not addressed. Just one crew member's impairment can result in increased burdens and fatigue on a small crew. If the conditions are left undetected, an impaired watchstander can have catastrophic consequences for the boat.
For advice on getting enough sleep while onboard, read Importance of Sleep While Boating (and How to Do It Safely).
What is Motion Sickness?
Kinetosis — commonly known as motion sickness — is any disorder caused by motion, such as seasickness, airsickness or carsickness, as defined by Taber's Cyclopedic Medical Dictionary. It is a common complaint of travelers on boats or planes, in motor vehicles, and even while riding animals such as horses.
Most people, including experienced boaters and frequent air travelers, have experienced motion sickness at some time. All that is needed is a strong enough stimulus, which can vary widely from one person to another. Most people acclimate — or 'get their sea legs' — with time, but the process can take up to two or three days.

Symptoms of Motion Sickness
The most distressing symptoms of motion sickness are nausea and vomiting, generally caused by an overstimulation of your inner ear's vestibular balance organs and/or by a discrepancy between the sensory inputs from your eyes and inner ears. Other symptoms include excessive sweating, pallor (pale skin), a mild headache and malaise.
Motion sickness is not a serious medical problem, but it may lead to more significant health issues or incidents because affected individuals can develop an almost desperate inattentiveness and a reduced ability to perform simple tasks. Assume that any tasks assigned to those affected by motion sickness require supervision. Reassign critical tasks to others who are less impaired.
Prevention and Treatment of Motion Sickness
It is best to plan ahead to reduce the risk of motion sickness. Prepare by being well-rested, nourished and adequately hydrated. If you feel anxious or uneasy, avoid consuming food for two hours before you embark for a short sail, as you will likely be more comfortable with an empty stomach than with a full one. For boaters, stow and prepare your gear before the boat leaves the dock to limit the time spent below decks.
While underway, position yourself on the boat where the motion is least, such as midline on the boat, low and close to the waterline or on the stern (if minimal or no exhaust is present). Avoid areas where the vertical motion is more pronounced, such as the bow or upper decks. Closing your eyes or sitting where the rocking motion of a boat is clearly visible can help prevent motion sickness. Gazing at the horizon rather than at objects in your immediate vicinity is widely accepted as helpful. Staying away from areas with strong fumes, particularly fuel or exhaust, is also a good idea. Avoid reading, looking at electronic devices or moving your head continuously back and forth because this can worsen symptoms.

Advertisements promote numerous medications, herbs, foods and devices to prevent or treat motion sickness. Although many of these aids have proved to be successful, none are known to be completely effective. Taking an over-the-counter antihistamine such as meclizine, dimenhydrinate or cyclizine before you feel sick can be helpful, but it may cause some degree of drowsiness. Antihistamines interact with many drugs, so if you have chronic health issues and are taking other medications, consult your physician before you travel so there is enough time to make any necessary adjustments. As always, it is wise to test new medications or supplements days to weeks before using them away from home. Motion-sickness medications typically are most effective when taken before symptoms begin and are less effective after symptom onset.

If necessary, motion sickness can be treated with either oral drugs or a transdermal patch, which delivers medication through the skin. On the rare occasion when nausea and vomiting are severe and not improving after several days and other problems begin to appear, the person may need to be returned to shore for medical attention.
Drugs used to prevent and treat motion sickness vary in their effectiveness and side effects from one individual to another, so it is not possible to make a generalized recommendation. Use such medications with caution during certain activities, as most of these drugs cause mild drowsiness and inhibit mucous secretions.
Motion sickness usually subsides as the body adapts or when the motion stops. Fortunately, the more frequently one travels, the easier it becomes to adjust to being in motion.
About Prescription Scopolamine
For many people, transdermal delivery of the prescription drug scopolamine can be effective. The patch, which goes by the brand name Transderm Scop®, contains 1.5 mg of scopolamine. When placed on the skin (typically just behind the ear), the patch delivers the drug at a constant rate for three days. Remove the patch after that period. Those who are still in an environment where motion sickness could be a problem can apply another patch. Wear only one patch at a time, even if you think one patch is depleted, to avoid too much medication entering the bloodstream and causing undesirable side effects.
Possible side effects of scopolamine include dry mouth, drowsiness, and blurred vision. Disorientation, memory disturbances, dizziness, and restlessness may occur but are less common. Scopolamine should be used with caution in patients with narrow-angle glaucoma, a pyloric obstruction or a urinary bladder neck obstruction (such as from an enlarged prostate). Rare side effects include hallucinations, confusion, difficulty urinating, skin rashes, and eye pain.
It is impossible to know in advance who scopolamine will affect and how. Therefore, before using a patch to prevent motion sickness, it is recommended to wear one on dry land for at least 24 hours to test its effects. Once you open the foil wrapper, avoid touching the patch under the plastic strip. If some of the medication gets on your finger and inadvertently contaminates your eye, the drug will produce unilateral pupil dilation, which has caused confusion with a number of serious medical emergencies by those who are unaware of this association. Do not consume alcohol while wearing a scopolamine patch.
If side effects occur, remove the patch. If you experience severe allergic reactions, difficulty urinating, pain in the eyes or dilated pupils, seek immediate medical attention.
If a patch is worn for more than three days, withdrawal symptoms can occur after removal. These symptoms, which generally do not occur until 24 hours after removal, include dizziness, nausea, vomiting, headache and balance disturbances.
Why Boaters Need a 'Plan B' for Motion Sickness
Whether you are planning an ocean crossing, a leisurely sail to the islands for a few weeks, or a day or two of deep-sea fishing, under certain circumstances motion sickness can be a potential hazard to recreational boaters.
Consider, for example, getting seasick while traveling offshore with your small children or your first bareboat charter vacation. In both cases, the severity of your symptoms could negatively affect your reaction times and your ability to concentrate. You may not be able to keep as close a watch on your kids' safety as you normally would. You may be too distracted to notice weather changes or objects lurking below the waterline. You may be unable to provide timely or appropriate assistance if someone falls overboard or gets injured. Many people with motion sickness will express that during the first few days of travel they experience apathy and a decreased attention to detail even if they never experience nausea or vomiting.
You cannot always anticipate the onset or severity of motion sickness, but with a bit of preparation, you can develop a plan to help manage the situation in case it occurs. Your 'Plan B' could be as simple as ensuring that someone else on board has the ability to take over or help when needed. If you are new to boating or if you are planning an expensive trip, consider taking a short, inexpensive day trip prior to your excursion, especially if it is one in which your best efforts are required for the safety of the trip. That way you have time to consider other options if you are susceptible to motion sickness.
The possibility of disordered sleep, watchstanding, inexperienced or rusty sailors, medications, and seasickness should require everyone to be vigilant and double-check themselves and each other.
What is Deep Vein Thrombosis?
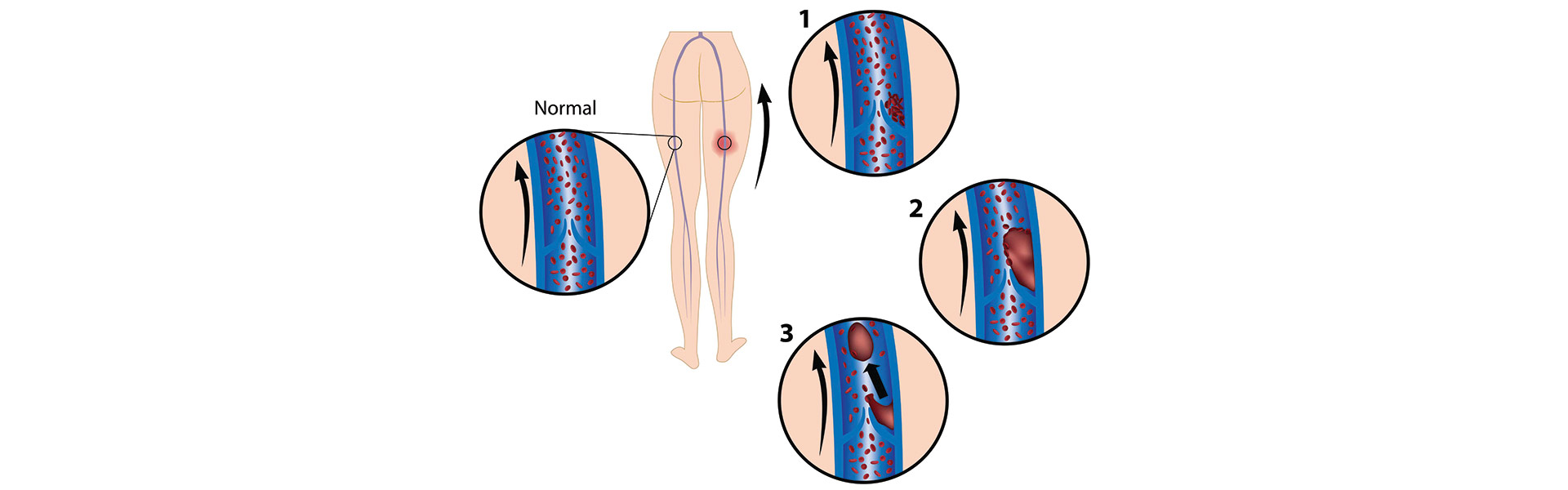
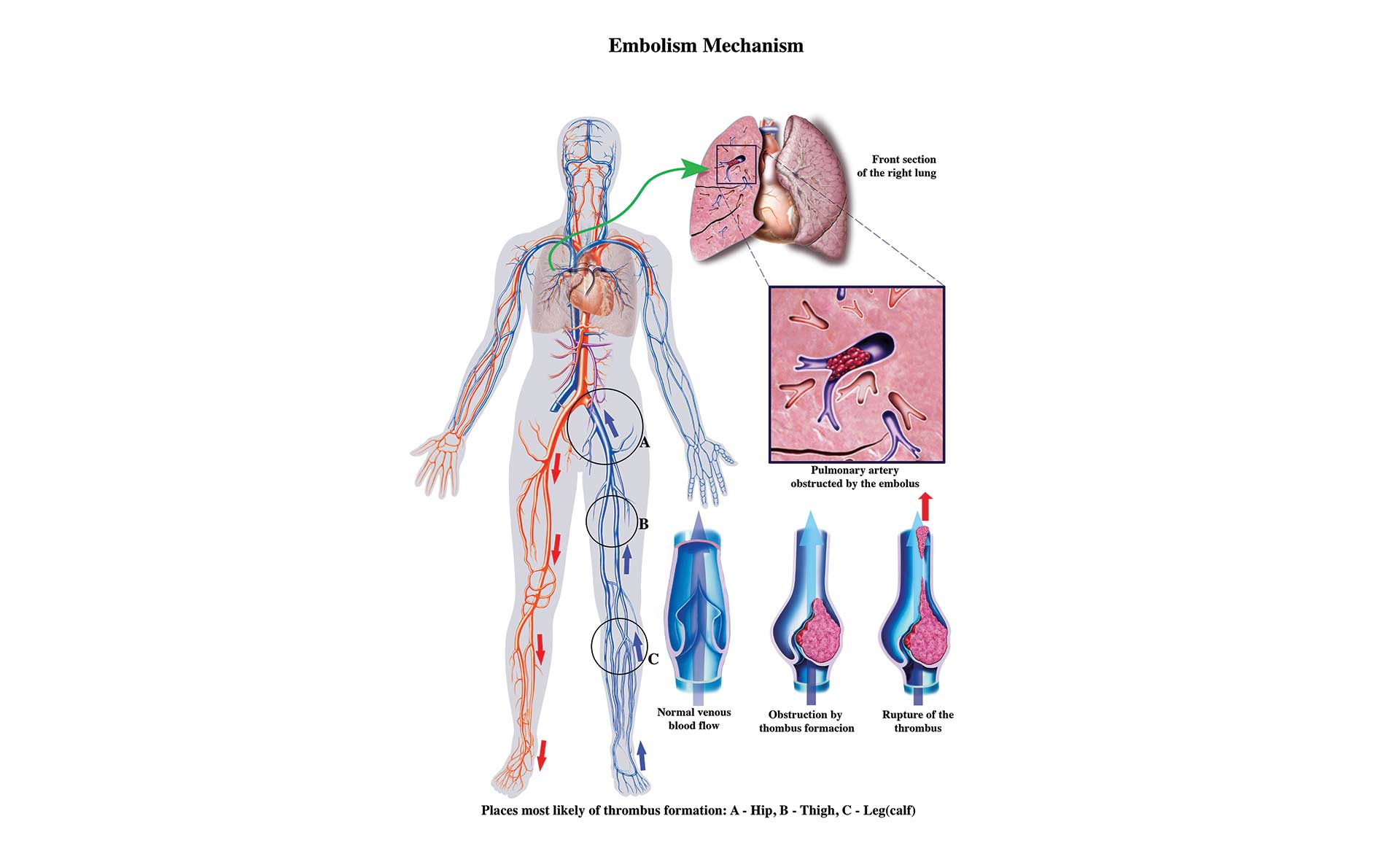
Deep vein thrombosis (DVT) is an acute condition in which a blood clot (also known as a thrombus) forms in one or more of the body's deep veins, usually in the legs. These blood clots can then break free, travel through the bloodstream and cause life-threatening conditions such as a pulmonary embolism — a blood clot that lodges in the lungs. The blockage can be great enough to reduce the heart's ability to circulate blood to the lungs, impairing vital functions such as the elimination of carbon dioxide and the delivery of oxygen.
Symptoms of Deep Vein Thrombosis
Approximately half of all DVTs are silent with no noticeable symptoms. When symptoms do occur, they may include the following:
- swelling of the affected leg, ankle, and foot
- pain in the calf that spreads to the ankle and foot
- warmth across the affected area
- change in skin color to pale, red or blue
These symptoms are not exclusive to DVT, and at least half of people with similar symptoms may have conditions other than DVT.
DVT often reoccurs and in many cases causes long-term complications such as postthrombotic syndrome (PTS) or pulmonary hypertension after a pulmonary embolism. PTS includes leg swelling, pain, skin discoloration and sometimes skin ulceration due to abnormal local circulation. It is caused by inflammation of veins and incomplete resolution of thrombi, which make veins less efficient at circulating blood out of the affected leg.
These complications can occur without a previous diagnosis of a DVT, which may be asymptomatic. Indeed, even when a DVT is suspected, its diagnosis is quite uncertain.
Travel is thought to increase the likelihood of a DVT. Most DVTs related to air travel occur within the first two weeks after a flight and resolve within eight weeks. In about 25 percent of cases, an untreated DVT of the calf can spread upward into the veins of the thigh and pelvis. If a DVT of the thigh or pelvis is left untreated, there is a risk of a blood clot that originated as a lower-extremity DVT moving centrally and lodging in a pulmonary vessel, resulting in pulmonary embolism. A massive pulmonary embolism is usually fatal.
About Pulmonary Embolism
Symptoms of Pulmonary Embolism include the following:
- sudden shortness of breath
- chest pain or discomfort that worsens with a deep breath or cough
- lightheadedness, dizziness or fainting
- rapid pulse
- sweating
- coughing up blood
- anxiety or nervousness
Pulmonary embolism is an emergency that requires immediate medical care. In remote locations, an emergency medical evacuation may be needed. In scuba diving situations, the diagnosis may be confused with dive-related injuries.
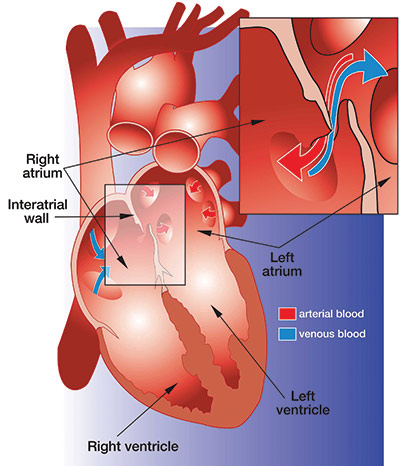
Another complication of a DVT is a condition called paradoxical embolism — in which a traveling blood clot passes directly into the arterial circulation instead of lodging in or being filtered through the pulmonary circulatory system.
Paradoxical embolism may occur in individuals who have a congenital condition such as patent foramen ovale (PFO) or atrial septal defect (ASD), in which a hole is in the wall separating the heart's right and left upper chambers — this enables venous blood to bypass the lung and pass directly to the arterial system. A clot that may have traveled from the calf to the heart through an atrial wall opening, for example, and into the arterial circulation is a paradoxical embolism. A paradoxical embolism that enters the brain may cause a stroke.
Prevention and Treatment of DVT

The risk of DVT in healthy, active people is small. Most cases of DVT occur in people with preexisting risk factors who are forced to sit still for a long time (such as travelers who take long plane, car, boat or train journeys), bedridden patients and office workers who sit at their desks for many hours. Immobility slows down the blood flow in the veins (a condition known as venous stasis), and pressure exerted on the calf by poorly designed seats can injure the vein walls. After sitting for 90 minutes, the blood flow in the calf drops by half, which doubles the chance of developing a clot. In individuals with preexisting risk factors, for every hour spent sitting, the risk of a blood clot increases by 10 percent.
The incidence of DVT in the general population is only 0.1 percent, but it is higher in high-risk subpopulations. Long-distance air travel — for which this condition is well studied — is thought to increase the risk of DVT two- to four-fold. The incidence for travelers on flights lasting more than four hours is between 1 per 4,650 flights and 1 per 6,000 flights. This risk is lower than for the general population because people who take long trips generally are healthier on average since very sick individuals tend to avoid long-distance travel.
After a trip of more than eight hours, the incidence of DVT among travelers with a low to intermediate preexisting risk for a DVT was found to be 0.3 percent for symptomatic cases and 0.5 percent when including asymptomatic cases. Again, remaining sedentary while traveling on a boat can share some of the same risks as those for air or motor vehicle travel.
DVT Risk Factors
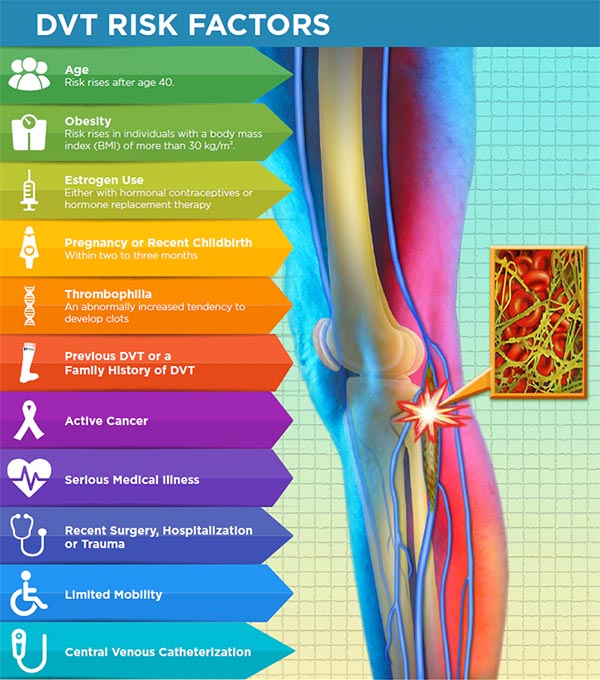
About 75 percent to 99.5 percent of individuals who develop a travel-related DVT have more than one of the following risk factors:
- age (risk rises after age 40)
- obesity (risk rises in individuals with a body mass index (BMI) of more than 30 kg/m2)
- estrogen use (either with hormonal contraceptives or hormone replacement therapy)
- pregnancy or recent childbirth (within two to three months)
- thrombophilia (an abnormally increased tendency to develop clots)
- previous DVT or a family history of DVT
- active cancer
- serious medical illness
- recent surgery, hospitalization or trauma
- limited mobility
- central venous catheterization
Airline passengers who are shorter than 5 feet, 3 inches (1.6 meters) or taller than 6 feet, 3 inches (1.9 meters) are at an increased risk of DVT because plane seats cannot be adjusted to their height. In addition to immobility, shorter passengers may experience seat-edge pressure on the backs of their knees, and taller passengers may be cramped due to insufficient legroom, increasing the likelihood of vein-wall injury, venous stasis, and activation of the blood's natural clotting mechanisms.
People with a predisposition to blood clots should wear compression socks (knee high) or stockings (thigh-high) when traveling and should consult their physician regarding the use of an anticoagulant medication such as aspirin.

Compression footwear reduces the chance that your blood will pool and clot, and anticoagulants inhibit your blood's ability to clot. Regular use of compression socks or stockings can also help prevent the swelling associated with DVT. It is usually advisable to wear compression footwear for at least a year after experiencing a DVT.
Anticoagulants (blood thinners) are drugs that inhibit your blood's ability to clot, thus reducing your risk of developing a clot. They range from over-the-counter medications such as aspirin to much stronger drugs such as warfarin (brand name Coumadin®) as well as newer direct oral anticoagulants. There is no evidence, however, that healthy people without preexisting risks for DVT benefit from compression footwear or anticoagulants.
People who cannot take anticoagulants, who have a DVT recurrence despite taking anticoagulants or who have repeated pulmonary embolisms can have a filter inserted in their inferior vena cava — the vessel that returns venous blood from the lower body to the heart. This filter, which is sometimes referred to as an umbrella because of its appearance, prevents clots that break loose from lodging in the lungs. Individuals with vena cava filters may return to a normal day-to-day life.
Everyone should avoid long periods of immobility — it is good practice to periodically get up and walk around while traveling. Exercising or flexing your feet and calf muscles while you are seated and staying well hydrated can also be helpful.
DVT is a serious medical condition that can result in death or major disability due to pulmonary embolism or PTS. Thus, it is an emergency that requires appropriate diagnosis and treatment to improve the chances of healing and to prevent life- and limb-threatening complications. In the hospital environment, early thrombus clearance rapidly resolves symptoms, preserves veins and restores their normal function.
Tips for Boaters on DVT
Most boat crews will be actively moving about the boat, completing their tasks for a successful voyage and minimizing such stasis. Some crew members may be immobile for prolonged periods due to physical condition or status, but this practice should be discouraged to mitigate the risk of DVT.
This information is applicable to a companion who remains seated next to a boat captain, who is standing at the helm, while the companion may be relatively dehydrated, sedentary, sitting with feet dangling and with pressure on the back of the thighs — a setup for a DVT.
On a boat, getting up and 'making rounds' not only may help prevent a DVT but also may help detect a problem with the boat early.
What is High Altitude Illness?
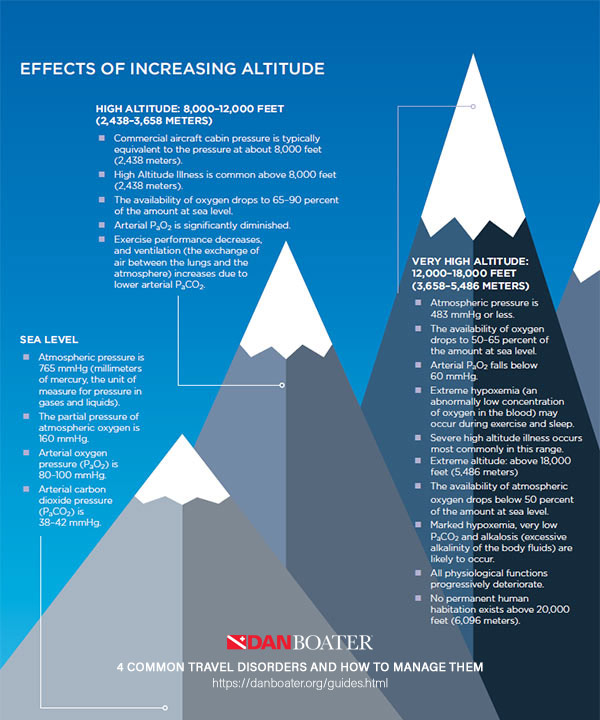
Traveling to high altitudes exposes people to increasingly rarefied air and progressively decreasing amounts of oxygen, resulting in declining levels of oxygen in the blood, which can lead to impaired physical and mental performance. Responses to high altitudes vary, but most people can function normally at heights up to 8,000 feet (2,438 meters) above sea level. At altitudes greater than that, the oxygen deficit can begin to cause a condition known as acute mountain sickness (AMS). At elevations higher than 10,000 feet (3,048 meters), 75 percent of people will experience at least mild AMS symptoms.
Symptoms of High Altitude Illness
The onset of AMS symptoms varies according to the altitude, the rate of ascent and the individual's susceptibility to the disease. A slow ascent may allow the body to acclimate by establishing a more rapid spontaneous breathing rate to make up for the decreased oxygen in the atmosphere. Symptoms usually start 12 to 24 hours after arrival at altitude and begin to decrease in severity around the third day at a given elevation.
AMS causes travelers to feel generally unwell. They may also experience a loss of appetite, headaches, lightheadedness, fatigue, breathlessness, rapid heartbeat, nausea or difficulty sleeping. Symptoms tend to be worse at night. Mild AMS does not interfere with normal activities, and symptoms generally subside within two to four days as the body acclimates.
Severe HAI manifests as serious conditions known as high-altitude pulmonary edema (HAPE) or high-altitude cerebral edema (HACE), caused by the accumulation of excess fluid in the lungs or brain. Symptoms of HAPE and HACE include a gray or pale complexion, a blue tinge to the skin (cyanosis), chest tightness or congestion, cough, coughing up blood, difficulty walking, shortness of breath when at rest, withdrawal from social interaction, confusion or decreased consciousness. These conditions can be fatal if not treated or if the victim is not returned to a lower altitude.
AMS Prevention and Treatment
Responding promptly to signs or symptoms of AMS is essential. Immediately call the nearest emergency medical services (EMS) if you or someone traveling with you experiences any of the following symptoms that could be HACE or HAPE:
- severe breathing problems
- altered level of alertness
- coughing up blood
If you cannot count on EMS aid, move the affected individual to a lower altitude as quickly and as safely as possible, and administer oxygen if it is available. Keep victims warm, and be sure they stay well hydrated if they are conscious.
To avoid high altitude illness, it is important to ascend slowly enough to allow time for your body to acclimate. Some people also find it beneficial to take prophylactic medication to help with the acclimatization process or to prevent some ill effects. If you plan to travel to a high-altitude location, visit your doctor or a travel clinic before your trip to evaluate your risk of HAI and to obtain prophylactic medication that may prevent or alleviate AMS.

Risk Factors for Acute Mountain Sickness
Anybody can be affected by AMS. Individuals who meet the following conditions are at a higher risk:
- You live at or near sea level and travel to a high altitude.
- You have had AMS before.
- You have preexisting medical conditions.
- You ascend quickly to a high elevation.
Consult your doctor before traveling to a high-altitude location if you have a heart, lung or blood disorder. You may need to travel with supplemental oxygen.

The following strategies can help prevent or moderate AMS:
- Ascend slowly above 8,000 feet.
- If you travel to high altitudes, choose a slow transportation method or walk.
- If you get there by flying, do not overexert yourself or travel still higher for the first 24 hours.
- If you travel above 10,000 feet (3,048 meters), increase your altitude by no more than 1,000 feet (305 meters) per day.
- After every 3,000 feet (914 meters) of elevation gained, take a rest day.
- After daily excursions, return to a lower altitude for the night, if possible.
- Do not go higher if you experience any AMS symptoms; wait for the symptoms to decrease before ascending.
- If your symptoms worsen, go to a lower altitude.
- Stay properly hydrated. Drink at least three to four quarts of fluids per day, and be sure to quench your thirst. Make sure to urinate regularly.
- Engaging in light activity during the day is better than sleeping, because respiration decreases during sleep, exacerbating AMS symptoms.
- Avoid tobacco, alcohol and depressant drugs (such as barbiturates, tranquilizers, and sleeping pills), all of which worsen AMS symptoms.
- Eat a high-carbohydrate diet while at altitude, but do not overeat.
- Boating and diving are not recommended.
HAI can affect those engaging in mountain climbing, mountaineering, rock climbing and hiking at higher elevations. Often these locations make medical evacuation difficult and delayed. Moving the victim to lower elevations becomes a priority for those who are accompanying the victim.

ABOUT DAN BOATER
Since its inception in 1980, DAN® has spent more than 300,000 medical resource hours on duty, fielding more than 100,000 emergency calls and coordinating more than 10,000 emergency evacuations worldwide, making it one of the world's most trusted resources for traveler safety.
As a natural evolution of DAN's successful 35+ years of service to the diving community, our new DAN Boater membership program is committed to helping recreational boaters in need of emergency assistance while traveling the globe, and to promoting smart travel health and safety practices through research and education.
By boat, plane, car, or rail. Around the world, or across the state. Anytime you travel more than 50 miles from home, rely on DAN Boater for the assistance you need when you need it:
- 24/7 Emergency hotline
- Medical information line
- Worldwide medical evacuation and repatriation services
- Search and rescue expense coverage
- Travel health and safety guides
- Global medical referrals, prescription assistance, and more
Learn how an affordable annual DAN Boater membership is helping thousands of travelers just like you every day.
Jet Lag Cure Lughts on Backs of Knees
Source: https://danboater.org/travel-health-and-safety/4-common-travel-disorders-and-how-to-manage-them.html
No comments:
Post a Comment